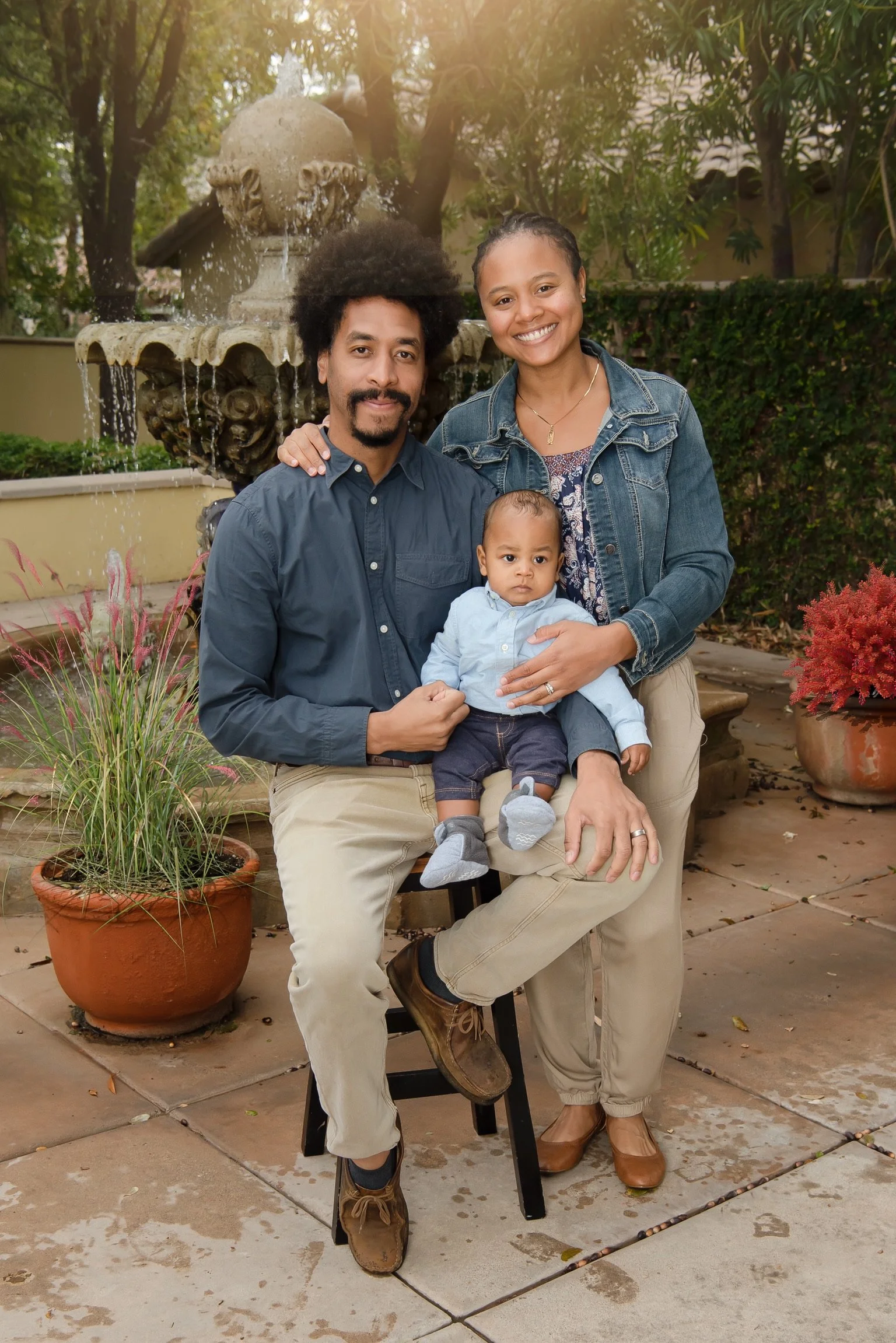
Yoga Instructor and traveling Occupational Therapist, Kelly Barnes shared her quicker than expected homebirth at 37 weeks. An experience she describes as "challenging, overwhelming, and rewarding all at the same time." Her expectations regarding when and how she would give birth were dismantled but the result was pure magic.
Kelly maintained an active lifestyle which included yoga and running throughout her pregnancy. Dual care with a certified homebirth midwife and OB. Envisioning a water birth was a focal point for Kelly as she embarked on her pregnancy. As a contingency, she enlisted dual care with a licensed professional midwife for the homebirth and an obstetrician to cover in case she needed to transfer from home.
Building up to her maternity leave, she loaded up on work to fully fund her maternity leave. As the nesting phase started to kick in she started to show signs of early labor. This sudden change caught Kelly off guard, and she wasn’t mentally or physically prepared for the baby to arrive. Her husband enlisted her sister to help her reconnect in mind and body to settle into the reality that she didn’t have weeks to prepare. Labor progressed as her husband scrambled to complete the homebirth checklist, thankfully, their doula was present to support her. The atmosphere shifted as her team slowly made their way to the home and set up the environment. Kelly managed labor with what was familiar to her, movement. She would live out her vision as she pushed her baby out.
Birth and motherhood are teaching Kelly that research is key, aligning with your care provider, and making informed choices.
Read More